 Most of us know that measuring a fasting blood glucose to assess how well someone is managing their glucose levels is about as crude and insensitive as waiting for the smoke detector alarm to tell you your dinner is cooked! If we wait to see an abnormal result here we’ve missed a prime opportunity for patient education and prevention long ago. Much the same story if you’re looking at HbA1c results.
Most of us know that measuring a fasting blood glucose to assess how well someone is managing their glucose levels is about as crude and insensitive as waiting for the smoke detector alarm to tell you your dinner is cooked! If we wait to see an abnormal result here we’ve missed a prime opportunity for patient education and prevention long ago. Much the same story if you’re looking at HbA1c results.
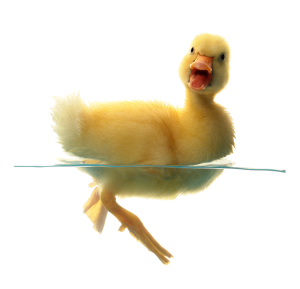
To explain this I always use the analogy of a duck. A duck will always be able to swim but the question is how much effort does it have to exert to swim the same distance? If your blood glucose is within range after an overnight fast that’s as good as saying, ‘this duck can swim the length of the pond’. What it doesn’t tell you is how fast its little legs are paddling in order to achieve that. Measuring a fasting insulin at the same time, however, tells us some additional important information. It tells you how fast the duck’s legs are paddling just to keep its head above water! The more insulin you’re having to secrete to just maintain normal blood glucose levels, the more alarmed we should be!
There has been much discussion about what constitutes a healthy insulin level but little consensus. Although the reference range in Australia for serum insulin is typically 5-20mU/L, informally most of us regard a fasting value of ≥10mU/L as too high. Other research proposes fasting serum insulin values ≥12.2 μU/mL, between meal values in the range of 8-11mU/L and post-prandial values over 50mU/L may constitute hyperinsulinemia and likely insulin resistance (Crofts et al 2015, see link below)
We were discussing this in a group mentoring session and someone asked about the HOMA-IR (Homeostasis model assessment for insulin resistance). This is a blood test offered by mainstream laboratories in Australia under subsidy, which measures both fasting glucose and insulin and then puts these results into a mathematical formula to anlayse the relationship between the two parameters.
Effectively, the HOMA-IR goes one step further and answers the question, ‘Should this duck be paddling this hard given how far it’s swum?’
The HOMA-IR is a well validated assessment of insulin sensitivity and can be used to diagnose insulin resistance, so if we’re trying to assess glucose handling competency in our patients why not measure the HOMA-IR and get the benefit of the added interpretation? You still get your insulin and glucose levels reported separately, so you can make your own findings from these, but an abnormal HOMA-IR creates a more clear cut and helpful talking point with the patient’s doctor.
Many thanks as always to the mentoring gang for keeping my brain ticking and to Claire for the link to this good review article on hyperinsulinemia which includes some discussion of BGL assessment https://diabesity.ejournals.ca/index.php/diabesity/article/viewFile/19/59
The Update in Under 30 audios which are recorded each month are now available via a 12 month subscription. These Mp3 juicy clinical soundbytes recorded by Rachel are less than 30 minutes and at under $14 per month, they’re a great way to stay up to date & earn CPE points on some of the most essential issues without leaving your desk!
