I’ve had my nose in all the research on Gilbert’s Syndrome again..watch this space…in the interim just thought I’d share this image and a couple of important details I may not have been able to convey when you last heard me talk (very fast!) about this important and common polymorphism:
- While the incidence is approximately 10% of Caucasian population, rates are heavily influenced by ethnic background and the highest rates (up to 1/4) are seen in Middle Eastern populations
- Gone are the days of thinking this condition only effects bilirubin levels and the enzyme responsible for its clearance – more recent research has shown over 3/4 of patients with Gilbert’s Syndrome have multiple SNPs that compromise clusters of enzymes within the glucuronidation pathway – with varying patterns – this goes a good chunk of the way to explaining the variability we see in bilirubin levels and symptom pictures across patients all deemed to have Gilbert’s Syndrome. This also explains why figures of reduced glucuronidation activity vary anywhere between 10% less to 90% less! It depends on your cluster..but the average reduction is around 50%
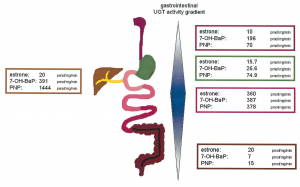
- UGT enzymes, the ones affected in Gilbert’s, are also expressed all the way down the GIT and constitute important food and drug handling. These UGTs are most active in the small intestines,as you can see above, but may explain why Gilbert’s patients are ‘more sensitive’ to medications than just paracetamol!
- And are you still thinking you need to run an $$$ gene test to confirm your Gilbert’s hunch in a client whose bilirubin sits consistently high normal or high? Think again… here’s a great little diagnostic short-cut that even the Royal College of Pathologists Australasia cites as sufficient evidence to confirm the polymorphism:
In the face of elevated total bilirubin levels and in the absence of liver pathology or increased haemolysis to explain this..”If the diagnosis is uncertain the serum bilirubin fasting level can be measured and should exceed the non-fasting level by >50%.”
Nice. So that means you only need to demonstrate that the patient’s fasting total bilirubin levels go up by at least 50% compared with their fed levels and BINGO you have your diagnosis. Much easier. Oh and this image comes from an interesting paper from Tukey & Strassburg 2001 – but is probably not for the faint-hearted 😉
Stay tuned for more 🙂
Just new to this condition and need a soft place to land with understanding Gilbert’s Syndrome? This previous UU30 is just the thing! Affectionately called Gilbert’s Girls because in particular it details a set of twins with this condition, this short audio explains the basics about this common polymorphism and why we tend to see a lot of patients who have this…even if no one has pointed it out to them yet! You could be the first to provide them with this important understanding about how genetics is impacting their detox pathways, changing their sex hormone handling and perhaps setting them up for both mental health issues and some serious upset guts! Better still, what to do once we have that diagnosis.