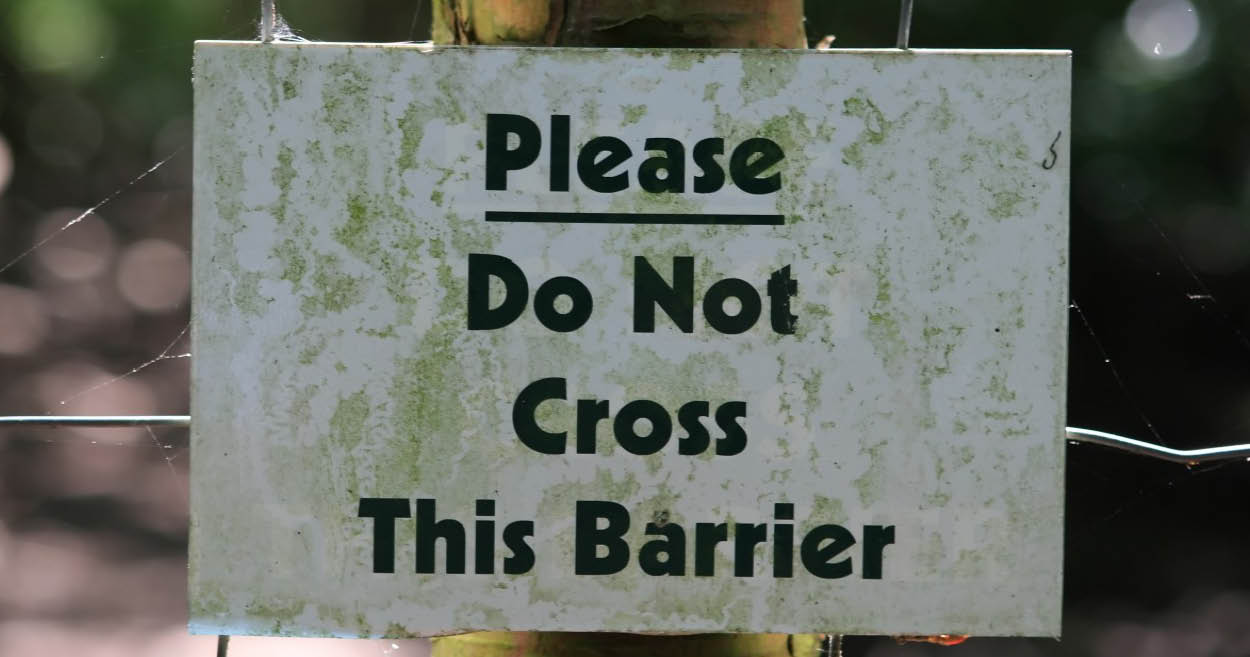
 Well that got tongues talking! We’ve cried, and we’ve laughed, hearing from practitioners about their ‘over-delivering donkey experiences’ for 2020. We’ve heard many memorable & relatable tales of either failures to set the best boundaries or even, in instances when we do, patients’ incredible dexterity to scale these in single leaps, ala James Bond style.
Well that got tongues talking! We’ve cried, and we’ve laughed, hearing from practitioners about their ‘over-delivering donkey experiences’ for 2020. We’ve heard many memorable & relatable tales of either failures to set the best boundaries or even, in instances when we do, patients’ incredible dexterity to scale these in single leaps, ala James Bond style.Practitioner: “On the very same day we talked about this important and ignored topic, I’d received an email at 9am from a patient asking for advice and a 2nd opinion about the prospect of surgery (first mention of this and clearly outside my scope!!!!), which they wanted before they saw the surgeon in 2 hours!!”
Sometimes it’s not patients, but professional colleagues (& friends)! I personally took an urgent call on Sunday morning from one of my psych colleagues, only because she is a dear friend, only to discover she needed help regarding a friend with mental health escalation…ah…yup…nup. Her blurred boundaries breached mine and then I bugged another colleague out of hours for further assistance…bad boundary blurring behaviour all round! We’ve been talking about the uncomfortable truth that a lack of healthy boundaries is a fast track to burn out for health professionals in group mentoring and the end of the year is always…opportune!
Mentee: “I felt challenged in a way where I was reviewing my own boundaries from an overall perspective over a period of time. I’ve worked in retail for 15 years now (as a student nat initially and then as a qualified naturopath) and I still find myself questioning how far I will go in certain respects especially when it comes to mental health (or people who appear vulnerable). When I was initially in practice I found my boundaries challenged to another degree, where I would accept every person who came through the door, whether I felt ready or not, or willing to take on the case, which essentially led me to burning out.Now as I get ready to start again in practice, I feel more prepared to set clear boundaries from the get go (give myself permission to do that) and check in with myself if I feel they are about to be crossed or not in alignment with me. It feels like an important and healthy assessment tool to utilise as a health care practitioner.”
As a profession we need to pool some solutions.
Instead of the reflexive, ‘Just pop me an email if you have any questions’, at the end of each consult which can constitute the equivalent of a blank cheque (!!), perhaps we can say, “If you need to clarify any advice I’ve given you today drop me an email and for any other questions that arise, we can decide whether we need to bring your next appt forward or schedule a between appointment phone consult” Or if you’re a practitioner who sees the value (and there is much research to support this) in increased touch points with patients, for better compliance and improved outcomes, then structure your billing accordingly. This from one of our cluey new grad mentees, ‘If you want to offer this add-on time as part of your service then you need to account for it e.g. shave 15 mins off the actual face to face time that they’ve been charged for, so as to have this ‘up your sleeve’ for this express purpose. They breed ’em smart these days! Love it!
The end of the year is such an important time for reflection. What have you learned this year about your professional boundaries? Got some tips you’d like to share?
**Reminder – Our 2021 Group Mentoring Program is opening soon!!!
Applications Open on 9th November!
Email [email protected] to let us know you are interested.
Applications Open on 9th November!
Email [email protected] to let us know you are interested.
